Picture this: your radiology department handles 500+ scans daily, and each image needs to reach the right specialist within minutes.
Manual routing creates bottlenecks, delays diagnoses, and frustrates both staff and patients.
Automated image routing based on study types and referral patterns changes everything by directing scans to appropriate radiologists instantly.
Modern radiology image sharing platforms now integrate sophisticated routing algorithms that analyze incoming studies and automatically distribute them according to predefined rules.
This technology reduces manual workload by up to 75% while ensuring critical cases reach specialists faster than ever before.
The Foundation: Study Type Classification
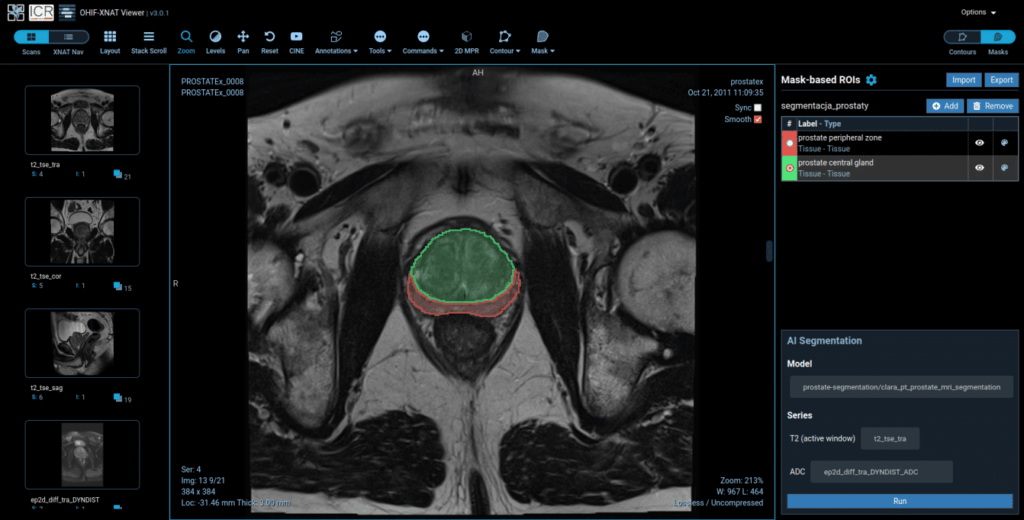
Your automated routing system starts with accurate study type identification. Most DICOM headers contain metadata that reveals exactly what type of scan you’re dealing with – whether it’s a chest CT, brain MRI, or cardiac ultrasound.
The system reads DICOM tags like Study Description, Series Description, and Body Part Examined to categorize each incoming image.
For example, when a chest CT arrives with “CHEST W/O CONTRAST” in the study description, the system immediately knows this belongs to thoracic imaging.
Advanced systems can identify over 200 different study types with 98% accuracy rates. They recognize everything from routine X-rays to complex interventional procedures, ensuring each scan lands in the right queue.
| Study Type | Average Processing Time | Specialist Required |
| Chest X-ray | 2-5 minutes | General Radiologist |
| Brain MRI | 15-30 minutes | Neuroradiologist |
| Cardiac CT | 20-45 minutes | Cardiac Imaging Specialist |
Referral Pattern Intelligence
Your system learns from historical referral patterns to make smarter routing decisions. If Dr. Smith typically handles all orthopedic cases from the emergency department, the system automatically routes those studies to her worklist.
Pattern recognition algorithms analyze thousands of previous cases to identify relationships between referring physicians, study types, and reading radiologists. This creates a dynamic routing matrix that adapts to your department’s unique workflow patterns.
The system tracks metrics like turnaround times, preferred reading patterns, and specialist availability to optimize future routing decisions. When your cardiac specialist is unavailable, it automatically redirects cases to the next qualified radiologist based on workload and expertise.
Setting Up Priority-Based Routing
Critical cases need immediate attention, and your automated system should recognize urgent studies instantly. Emergency department scans, stroke protocols, and trauma cases get priority routing to available specialists within seconds.
You can configure priority levels based on multiple factors:
- Referring department (Emergency = High Priority)
- Clinical urgency indicators in study descriptions
- Patient age and condition from DICOM metadata
- Time-sensitive protocols like stroke alerts
Most systems allow you to create custom priority rules. For instance, any brain CT ordered between 6 PM and 6 AM automatically receives urgent status and routes to the on-call neuroradiologist.
Workload Distribution and Load Balancing
Fair workload distribution prevents radiologist burnout while maintaining consistent turnaround times. Your routing system should monitor each radiologist’s current queue and distribute new cases accordingly.
Smart load balancing considers several factors:
- Current number of unread studies per radiologist
- Complexity of pending cases (a cardiac MR counts more than a chest X-ray)
- Individual reading speeds and preferences
- Scheduled breaks and shift patterns
When one radiologist has 15 pending studies and another has 5, the system routes new cases to the less busy colleague. This maintains workflow balance throughout the day.
Integration with Existing Systems
Your automated routing connects seamlessly with PACS, RIS, and worklist management systems. Most modern platforms offer HL7 FHIR APIs that enable real-time communication between different healthcare software.
The integration process typically involves mapping your current workflow rules into the routing engine. You’ll need to identify all possible study types, define specialist assignments, and establish priority protocols.
Implementation usually takes 2-4 weeks, depending on system complexity and customization requirements. During this period, you can run parallel workflows to ensure accuracy before entirely switching to automated routing.

Measuring Success and Optimization
Track key performance indicators to measure your routing system’s effectiveness. Average turnaround times typically improve by 40-60% after implementing automated routing.
Important metrics include:
- Study distribution accuracy (target: >95%)
- Turnaround time reduction
- Radiologist satisfaction scores
- Routing errors and corrections needed
Monitor these metrics monthly and adjust routing rules as needed. Your system should evolve with changing department needs, new specialists, and updated protocols.
Most successful implementations show immediate improvements in workflow efficiency while significantly reducing administrative overhead.